Cervical cancer was once one of the leading killers among gynaecologic cancers in the western world but this trend has been reversed through the combined efforts of improved screening, early treatment and vaccination. Unfortunately, the trend still persists in Sub-Saharan Africa. In Nigeria, it is responsible for the second highest number of cancer deaths in women only behind breast cancers. World wide statistics make it the fourth leading cancer in women with most of the deaths from this cancer occurring in low and middle income countries.
Other common cancers that affect women are endometrial, ovarian and vulva cancers.
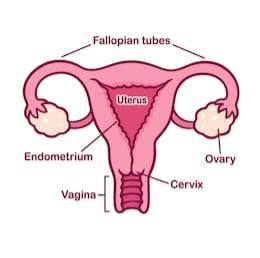
What is Cervical Cancer?
Cervical cancer are abnormal growth cells at the opening of the womb. Like every other cancer, the cells grow abnormally, at an abnormal rate and may invade surrounding tissues.
Most cases of cervical cancer are caused by some types of the Human Papillomavirus (HPV). There are more than 100 types of HPV and over 14 cause diseases with type 16 and 18 causing most of the cases as high as 70%. They are also associated with anal cancers, oropharyngeal, vaginal and penile cancers.
HPV is mostly sexually transmitted and is usually contacted within the first few exposures and does not require penetration for transmission (genital skin contact is enough for transmission).
Risk Factors
Some of the risk factors include the infection with HPV and the sub-type of HPV infection present.
Early coitarche – early first sexual exposure – increases the risk of getting the virus and thus there is a longer period of possible exposure and concomitant risk of having cervical cancer.
Co-infections such as HIV reduces immunity to fight off the HPV.
Multiple sexual partners increases both the chance and load of viral infection.
Natural History
Most cases of HPV infection clear without any sequelae. The few that progress over the next 10 to 15 years may progress to precancerous (before cancer) lesions know as Cervical intraepithelial Neoplasia(neoplasia means development of abnormal cells. There are 3 stages:
CIN 1 affects about one-third of the thickness of the epithelium, these are less likely to become cervical cancer but may progress to CIN2.
CIN 2 affects about one-third to two-thirds of the epithelial layer, with a 5% chance of becoming cervical cancer.
CIN 3 affects more than two-thirds of the epithelium and stands at about 12% risk of progression.
Carcinoma insitu is when the neoplasm has extended to the whole epithelium.
Prevention of the Disease
Since the commonest cause is prolonged infection with HPV, the simplest way would be to stop the infection. This can be done by complete abstinence from sex (highly unlikely) or protected sexual intercourse. Fortunately, there are vaccines available for prevention of HPV serotypes that cause the disease.
These vaccines work best given before coitarche, thus WHO recommends giving girls between 9 and 14. Some countries have also started vaccinating young boys as they are potential spreaders of the virus later on in life. Women of reproductive age should also take the vaccine even if they have started having sex, they just need to screen prior to the vaccine.
The next step of prevention is regular screening. This includes:
1. A visual examination with acetic acid and lugols iodine, commonly done in resource poor communities. Here the cervix is examined by a trained health care provider for reactions of the neoplastic cells to Acetic acid and lugols iodine. This only takes a few minutes and if positive treatment can be given immediately. At this point, a small piece of the cervix can also be taken for a biopsy to confirm the diagnosis.
2 HPV DNA screening is done in centers with the facilities and can specifically identify the presence of the viral sub-types.
3 Pap’s test is done by scrapping the cells of the cervix with a soft brush and then an examination of the scrapings is done to check for precancerous cells.
Treatments
For the precancerous lesions, available options include cryotherapy, loop electrosurgical excision procedure(LEEP) and thermal ablation.
More advanced disease needs to be further investigated and staged. Treatment includes surgery, chemotherapy and radioterapy. Palliative care is also given in disease with unfavorable prognosis.
The most used staging method is graded I to IV with the latter being most advanced. Criteria are size of lesion, local spread and nodal metastases.
Conclusion
Cervical Cancer is one of the few vaccine preventable cancers and also has a long transition period with multiple stages of intervention before the onset of the worst phase. As such, we have a rare opportunity to eradicate or minimise the burden of disease. This is not just a WHO campaign, but a community based problem and individual battle. We all have our parts to play in raising awareness, getting screened and vaccinated.